Endodontics (root canal treatment) is a specialised branch of dentistry that is involved in the health and disease of the dental pulp and 'root canal' space (which contains the pulp tissue) and surrounding (periapical) tissues and with the prevention, diagnosis and treatment of diseases and injuries in these tissues.
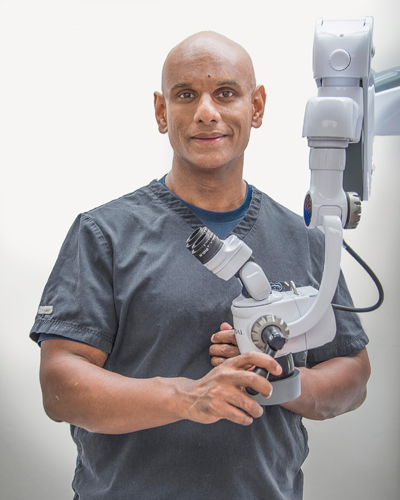
Although General Dentists can perform Endodontic treatment, patients are often referred to an Endodontist when the case is complicated or more difficult than usual. At The Park Clinic we are very fortunate to have Specialist Endodontist Dr. Rohan Rajasingham who is expert at treating such complicated cases.
An Endodontist is a dentist who has undergone extra postgraduate specialist Endodontic training. In the UK, admission to the Endodontic Specialist List and the status of Specialist in Endodontics is given by the General Dental Council of Great Britain and N.Ireland after a rigorous assessment procedure.
Specialist training allows an Endodontist to:
Your general dentist sometimes refers patients for consultation when the diagnosis is complicated or when treatment is more difficult than normal.
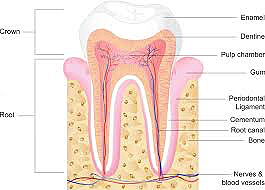
Inside the tooth, under the white enamel and a hard inner layer called the dentine, is a soft tissue called the pulp. The pulp contains blood vessels, nerves and connective tissue. The pulp extends from the crown of the tooth to the tip of the roots where it connects to the tissues surrounding the root. The pulp is important during a tooth's growth and development. However, once a tooth is fully mature it can survive without the pulp.
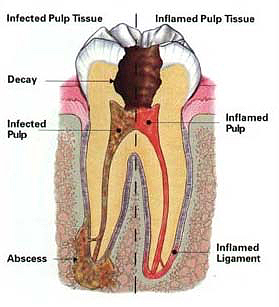
There are approximately 500 different species of bacteria that can normally be found in the mouth. These bacteria, when given the opportunity, are responsible for causing the dental diseases such as caries ('decay'), periodontal ('gum & bone') disease and endodontic ('root canal') infections. The pulp can get inflamed or, in the worst cases infected, when the tooth's natural defences (the hard enamel and reparative pulp-dentine) are breached. The usual causes of such breaches are deep decay, repeated dental procedures on the tooth, or trauma to the tooth.
The pulp is a delicate organ and very often does not survive multiple injuries by bacteria, heat or chemical irritation (usually from filling materials). With mild irritation the pulp may just become inflamed and if managed early enough, the inflammation can be reversed. However, when the pulp 'dies', the resulting infection becomes established inside the root canal and may lead to an abscess in the bone. At this point, the tooth may either be extracted or saved by carrying out root canal treatment (Endodontic treatment).
Signs of pulp damage include pain, prolonged sensitivity to heat and cold, discolouration of the tooth, and swelling and tenderness in the nearby gums. Occasionally there are no symptoms and you may be completely unaware that there is a low-grade underlying infection in the tooth.
The endodontist will remove the inflamed or infected pulp, carefully clean and shape the inside of the tooth, and then will fill and seal the space. When there is an infection inside the canals it is likely to cause discomfort or pain at some time. The infection may cause the formation of an abscess, which can then result in a facial swelling. Root canal treatment will remove the cause of the pain, and allow your own body's defences to heal the area.
Afterwards, you will need to return to your own dentist, who will place a crown or other restoration on the tooth to protect and restore it to full function. After restoration the tooth will continue to function like any other tooth.
Front teeth are likely to have just one canal, but further back in the mouth teeth will have three, four or sometimes even five canals.
The specialist endodontist uses a high magnification microscope to aid location of the canals and enables the endodontist to carry out all aspects of root canal treatment/retreatment to the highest possible standard.
A treatment appointment is likely to last for 1.5 to 2 hours. Low dose x-rays are used as necessary.
Many root canal treatments are performed to relieve the pain of toothaches caused by pulp inflammation or infection. It is unlikely that you will feel any discomfort – a combination of gentleness and effective local anaesthesia usually ensures a comfortable experience.
For the first few days after treatment your tooth may feel sensitive, especially if there was pain or infection before the procedure. This discomfort can usually be relieved with over the counter medication (analgesics such as Ibuprofen). Very rarely, antibiotics may need to be prescribed.
Every root canal treatment is specific to a patient and the complexity of a root canal treatment will vary considerably depending upon a number of factors. These will also influence the number and length of visits that will be required. Some treatments will only require one visit and some will require several. Following referral by your general dentist, the endodontist will be able to give you an indication of the number and length of visits and of the approximate cost prior to you attending for treatment.
You should be careful when biting or chewing on your tooth until you have had it restored by your dentist. The unrestored tooth is susceptible to fracture, so you should see your own dentist for a full restoration as soon as possible.
Most endodontically treated teeth can last as long as other natural teeth. In a few cases, a tooth that has undergone endodontic treatment fails to heal or the pain continues.
Some patients may have had previously unsuccessful root canal treatment. The usual reasons for failure are either because one or more canals have been missed, or because the root fillings do not extend right to the tip of the roots as they should. This would allow infection to remain inside the tooth, which over time will likely cause pain and/or swelling.
Patients may often be referred for root canal treatment if restorative treatment is needed to a particular tooth and the general dentist wants to be sure that the root will not give problems later. It would, for example, be unwise to crown a tooth which had signs of a potential root tip infection. In such a case first ensuring the viability of the root will ensure the long-term future of the crown.


"Our aim is to help our patients keep their teeth and gums healthy by giving them the best possible professional treatment and advice. However any type of periodontal treatment requires that the patient continues to observe good daily care at home." Dr. Pradeep Nair